*Fine-Tuning Breath Deli...

Highlights
- Fine-tuning breath delivery to maximize CO2 elimination in ARDS
1/
In these testing times, I've resorted to learning new concepts to distract myself. Sharing something I learned recently due to its current relevance.
(Discussion is limited to passive mechanical ventilation) (View Tweet)
- 2/ Why does CO2 elimination matter in ARDS?
Enhanced CO2 elmination would allow reduction of delivered minute ventilation (and hence, VILI).
The question I had was, is there's something that can be done to maximize CO2 removal for a given tidal volume and RR. The answer is yes. (View Tweet)
- 3/ There are, in fact, 2 major strategies:
(i) Minimize apparatus dead space (VDapp)
(ii) Modulate breath delivery (which ultimately reduces airway/anatomical VD)
(i) Practically, any component distal to the Y-piece contributes to VDapp. More on this -
https://t.co/EmfMbeJRJW (View Tweet)
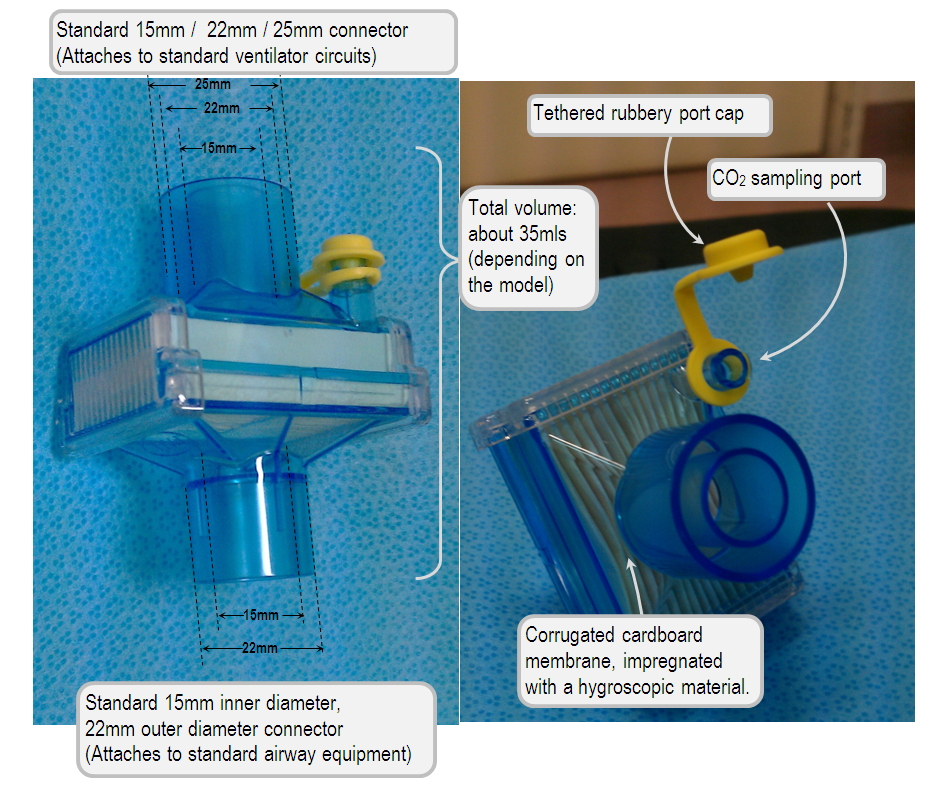
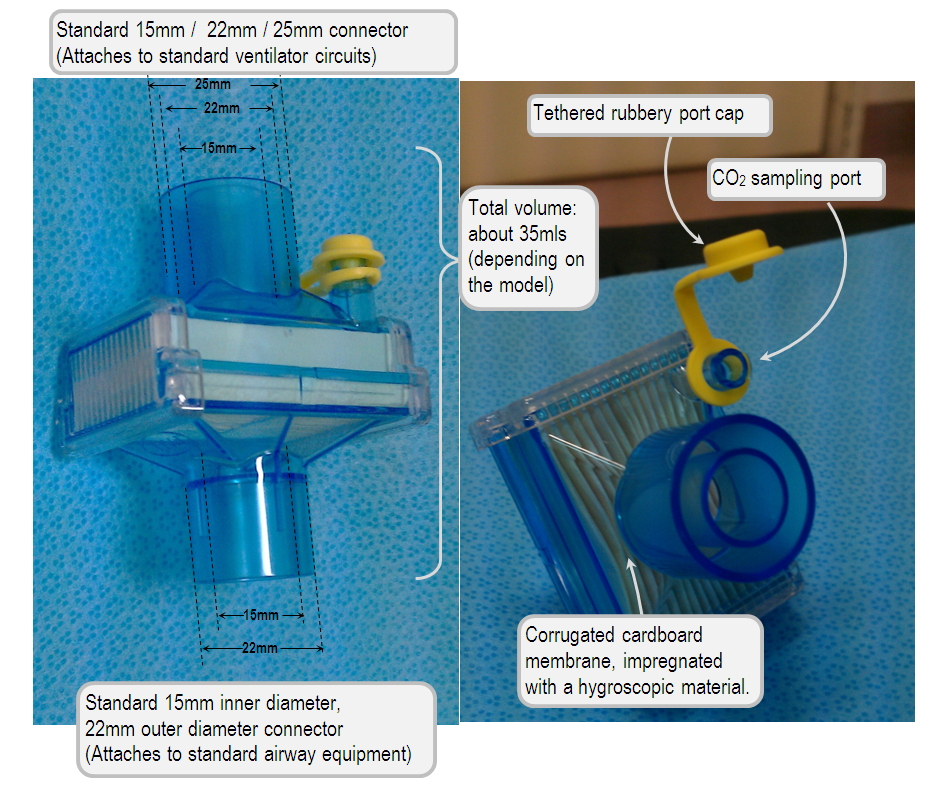
- 4/Apart from the occasional extension tubing, the most common culprit for VDapp is a passive HME. These may cause anywhere from 35cc to 90cc of VDapp
(see: https://t.co/EV7KGqZYCY)
This can be overcome by using active circuit humidification (luckily, this is default in our MICU)
 (View Tweet)
(View Tweet)
- 5/ (ii) Now the fun part. There are 2 factors of breath delivery that enhance CO2 elimination:
(a) Mean distribution time (MDT): more important (image)
(b) End inspiratory flow (EIF) rate: variable importance
(a) The idea behind MDT is that diffusion is a time dependent process.
 (View Tweet)
(View Tweet)
- 6/ A longer MDT allows more time for gas exchange with every breath. For a fixed I:E ratio, MDT can be significantly increased by using a post-inspiratory pause while reducing the insufflation time (image).
(b) A high EIF may help as higher flow transients at airway opening are
 (View Tweet)
(View Tweet)
- 7/ are better transmitted to the periphery. However, this effect varies with the underlying lung mechanics (particularly compliance) so is not robust.
Clinical studies - in PMID: 27558174, they were able to reduce TV from by ~42cc (6.3 to 5.6/kg IBW) for the same resultant pCO2. (View Tweet)
- 8/ These numbers may seem trivial but they become important when we're shooting for the lowest possible TV
Although I'm a strong proponent of permissive hypercapnea, this may become a problem in certain situations (most commonly in acute cor pulmonale where CO2 may drive up PVR) (View Tweet)
- 9/ E.g. Baseline settings = TV = 400 (8cc/kg), RR = 30. Gas exchange acceptable. Can't raise RR further due to auto-PEEP.
You notice this patient has an HME with VDapp = 50cc. Plus you realize you may able to squeeze an additional 50cc by utilizing a post-inspiratory pause. (View Tweet)
- 10/ So by simply removing the passive HME (switch to inline) and adding a post-inspiratory pause, TV can potentially be reduced from 400 to 300 with no change in pCO2.
I recently had an N=1 experience that was in line with this discussion. Curious about other thoughts on this. (View Tweet)
- @emireles_c @msiuba @roeckler @DrivingPressure @curso_vm @medevidenceblog @ogi_gajic @donnatanner815 @respresource @SMHCoEMV (View Tweet)

 (View Tweet)
(View Tweet) (View Tweet)
(View Tweet) (View Tweet)
(View Tweet)